From Scott’s blog Semaglutidonomics
140 million obese Americans x $15,000/year for obesity drugs = . . . uh oh, that can’t be right.
I don’t think anything short of drastic medical intervention, such as Semaglutide, or a major disruption of society (e.g societal collapse or famine) can put a dent in the worldwide obesity/overweight epidemic. Or if not Semaglutide, stimulants such as Phentermine, which is cheaper and in the mid 20th century was readily available and commonly used for weight loss, and still is prescribed. Unlike Phentermine, Semaglutide is meant to be taken long term and has fewer potential adverse side effects.
Of six major weight loss drugs, only two – Wegovy and Qsymia – have a better than 50-50 chance of helping you lose 10% of your weight. Qsymia works partly by making food taste terrible; it can also cause cognitive issues. Wegovy feels more natural; patients just feel full and satisfied after they’ve eaten a healthy amount of food. You can read the gushing anecdotes here (plus some extra anecdotes in the comments). Wegovy patients also lose more weight on average than Qsymia patients – 15% compared to 10%. It’s just a really impressive drug.
10-15% is easily enough to turn an obese person only overweight, or an overweight person ‘normal’ (which if 75% of the country is overweight or obese, is it still normal?).
As discussed earlier, the obesity epidemic is possibly more resilient to lifestyle modification than commonly assumed, because for people with mediocre or poor genes (e.g. slow metabolism, overproduction of ghrelin, poor exercise tolerance and response to training [0], or low muscle mass), specially after the age of 30 when metabolic slowdown and gradual muscle loss occurs, that nothing short of near-starvation diets and or hours of exercise/day will make these people normal weight, which is an impractical solution for people with jobs and families.
Economic productivity would probably fall if tens of millions of people had to subsist on borderline starvation rations [1], while feeling hungry and probably irritable and fidgety all the time, and still allocating enough time for hours of daily exercise while working. The loss of economic productivity would probably to some extent negate the reduction of healthcare costs of less obesity-related healthcare spending. Food isn’t just for satiety but also acts as a stimulant.
Consider that someone can have favorable or unfavorable genes (such as for metabolism), and either enjoys or dislikes exercise. Someone who enjoys exercise is more likely to make a habit out of it than someone who doesn’t. So there are four possibilities:
Good genes, enjoys exercise
Bad genes, enjoys exercise
Good genes, hates exercise
Bad genes, hates exercise
Those in the last category are guaranteed to be obese. Those in the second or third categories are likely to at least be overweight. Those in the first category can probably stay thin, without weight gain later in life. Assuming each possibility is equally probable, 75% of the population has an unfavorable combination, which is very close to the percentage of Americans who are at least overweight, 74%. Exercise intolerance is likely also genetic, and some people are destined to be poor at cardio, which is evident even as early as childhood. Indeed, in my high school gym glass, approx. 1/4 of the class was unable to run a mile, 50% could do it (but unenthusiastically or at a poor/mediocre time), and the remaining 25% could run it at a good time and seemed to enjoy it. Again, we see a similar 25-75 ratio. The 25% who are good at running and enjoy it are likely to make it a habit, and hence stave off becoming overweight or obese later in life.
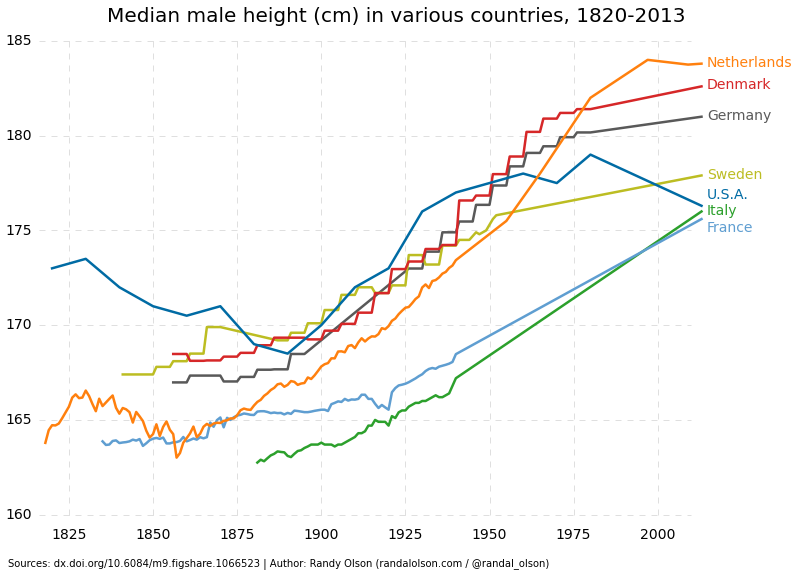
It also does not help that people are getting bigger overall, not just wider, but taller. Via the square-cube law of scaling, a one-percent increase in height corresponds to a 3% gain in weight, which is good for weightlifting, but makes it harder to do cardio, which is more effective in terms of calories burned/hour than weightlifting.
It’s even worse when you include ‘skinny fat’ syndrome, which describes people whose BMIs may be normal or only slightly overweight but who still pack a lot of abdominal fat.
Of course, a common rebuttal is that people seem fatter today compared to generations ago. How does one reconcile abrupt phenotypic changes with gradual genomic changes. I think some of this can be explained by adiposity being underreported/undiagnosed in the past, not that people are getting fatter, although that too plays some role. [Sedentary lifestyles and processed, caloric-dense foods are important contributors.] This explanation deserves much more consideration. [2] There were plenty of fat people 50-80 years ago, but as doctors and patients became aware of the problem, it led to more people being diagnosed. [If you are looking for something, you are generally going to find more of it.]
Also, plenty of overweight or obese people do not look like they are fat, such as due to baggy or loose-fitting clothes, unless they take their shirt off, so photos from the 50s-70s of alleged slimness may be deceiving. Your average obese person does not look like a contestant of ‘The Biggest Loser’, but may have a slightly protruding stomach, which is enough to have a BMI of 35+ even if it’s not that overtly obese. For example, my BMI is technically in the overweight category, 25-26 or so depending if I round my height up or down to the nearest inch, yet if I was transported back to the 1950s and photographed wearing the attire that was common at the time, no one today would look at that photo today and be like, ‘Wow that guy is overweight!’
If people were so thin 70+ years ago, why was phentermine developed in the first place? Obviously, there was a demand. The weight loss industry was big even in the 1950s. There were fad diets in the ’50s, too, like we see today. Americans have been trying to lose weight, unsuccessfully, for a long time. Maybe a new generation of weight loss drugs, such as Semaglutide and Wegovy, will change this. Let’s hope something works!
[0] Genes play key role in exercise outcomes.
A new study has found that genes can explain up to 72% of the difference in outcome between people after a specific fitness exercise. The research involved data from 3,012 adults and has identified a number of specific genes which influence the outcomes of different physical activities.
[1] It’s not hyperbole when I say starvation-level rations. For example, to stay slim reverend Al Sharpton eats only 1,000 calories/day, half the recommended guidelines of 2,000 calories/day. This amounts to two juices, two bananas, a salad, and three pieces of toast.
At my desk at NAN Corporate during my daily staff briefing. I have a salad mid morning, 3 slices of full grain toast (no butter or jam) and one banana. That’s my daily intake. I feel GREAT and workout before dawn every morning. pic.twitter.com/2V3sT725dL
— Reverend Al Sharpton (@TheRevAl) July 31, 2018
This is 350-650 fewer calories than predicted by a BMR calculator (age 68, weight 130, height 5’10”). Crazy. Good luck getting all 200+ million overweight or obese Americans complying with such a diet.
[2] From what I can glean of paintings of the Founding Fathers, at least 1/3 of them appear to be in the obese or highly overweight category, almost similar to today, but this was in the 1700s, long before the advent of processed foods and junk food. This suggests relatively high rates of adiposity long before it became a public health problem, which goes against almost every narrative about the topic.

Few of these people seem thin.
If the recommended caloric intake makes 75% of the population overweight, than the recommendation is by definition incorrect